Gabapentinoids as Perioperative Analgesics
Gabapentinoids have been approved for treatment of neuropathic pain for conditions such as spinal cord injury or post-herpetic neuralgia1. This class of drugs includes gabapentin and pregabalin. With growing concern over the current opioid epidemic, use of gabapentinoids has increased drastically to decrease prescription of opioids and to reduce acute and chronic pain after surgery2. The American Pain Society supports the use of gabapentinoids in the perioperative period, but more recently, researchers have shown skepticism toward the efficacy of gabapentinoids.
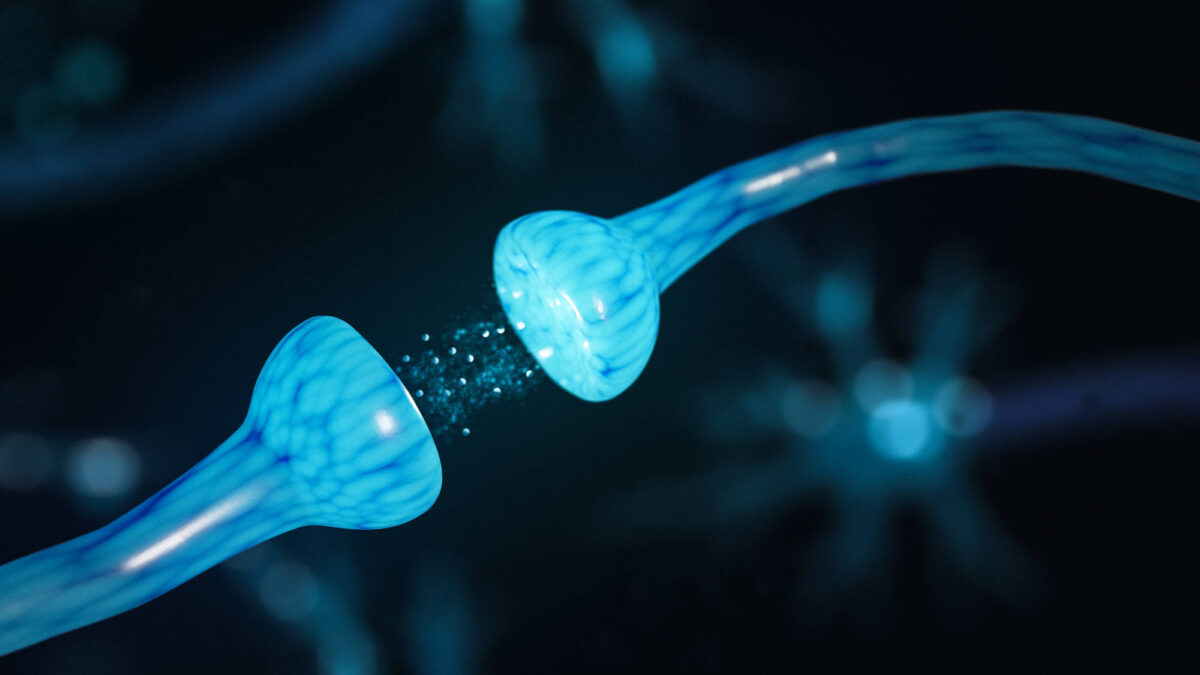
Gabapentinoids, structural analogs of γ-aminobutyric acid, bind to presynaptic voltage-gated calcium channels and regulate the release of excitatory neurotransmitters. Specifically, these compounds inhibit glutamate release from pain-transmitting neurons, decreasing pain signals3. Gabapentin absorption takes place in a limited area in the duodenum, and pregabalin absorption takes place in the small intestine. Both drugs exhibit similar adverse effects, including dizziness, headache, visual disturbances, and peripheral edema, but trial results indicate that gabapentinoids are generally well-tolerated4.
A study conducted by Khan et al. studied patients who received gabapentin before and after lumbar laminectomy. Patients reported lower pain scores at every time point within the first 24 hours when receiving 900 or 1200 mg of gabapentin compared to placebo or 600 mg of gabapentin5. Another study also exhibited positive correlation between higher dosage of gabapentinoids and higher efficacy. The results showed that higher doses of gabapentin (900-1500 mg) more effectively reduced pain and opioid use after surgery6. Buvanendran et al. administered either placebo or 300 mg pregabalin to patients before their knee replacement surgeries. Patients in the pregabalin group reported little or no postsurgical chronic pain after three months, while 8.7% of patients in the control group reported pain7. Research conducted on pregabalin and gabapentin indicate similar pain reduction potential; however, there is more research on gabapentin, and gabapentin is more cost-effective.
However, more recent research indicates that researchers are no longer confident in the efficacy of gabapentinoids. Verret et al. published a study this year that included 281 trials in a meta-analysis. The study focused on the intensity of postoperative acute pain, cumulative opioid use, and adverse events. Contrary to previous studies, Verret pointed out that there should be a minimally important difference threshold for pain intensity, which was set at ten points in a pain intensity scale out of 100. Out of 24,682 participants, the average difference in pain intensity between the gabapentinoids and control groups was below ten points, which was below the statistically significant difference threshold. This pattern was evident at 6, 12, 24, and 72 hours after surgery. The gabapentinoids group did not exhibit more adverse events than the control group. On average, gabapentinoids reduced postoperative nausea and vomiting, but increased incidence of dizziness. This most recent study concluded that gabapentinoids did not exhibit any clinically significant benefits as perioperative analgesics.2
Past study results have encouraged the use of gabapentinoids both preoperatively and postoperatively. Off-label use of pregabalin and gabapentin has increased in the past decade due to fear of opioid abuse. Recent stances on gabapentinoids have become unclear, as more researchers begin to question its efficacy. Future research should attempt to answer discrepancies between past and present research.
References
- 1. Peter C. Schmidt, Gabriela Ruchelli, Sean C. Mackey, Ian R. Carroll; Perioperative Gabapentinoids: Choice of Agent, Dose, Timing, and Effects on Chronic Postsurgical Pain. Anesthesiology 2013;119(5):1215-1221. doi: https://doi.org/10.1097/ALN.0b013e3182a9a896.
- 2. Michael Verret, François Lauzier, Ryan Zarychanski, Caroline Perron, Xavier Savard, Anne-Marie Pinard, Guillaume Leblanc, Marie-Joëlle Cossi, Xavier Neveu, Alexis F. Turgeon, the Canadian Perioperative Anesthesia Clinical Trials (PACT) Group; Perioperative Use of Gabapentinoids for the Management of Postoperative Acute Pain: A Systematic Review and Meta-analysis. Anesthesiology 2020;133(2):265-279. doi: https://doi.org/10.1097/ALN.0000000000003428.
- 3. Weinbroum, AA Non-opioid IV adjuvants in the perioperative period: Pharmacological and clinical aspects of ketamine and gabapentinoids. Pharmacol Res. (2012). 65 411–29
- 4. Zhang, J, Ho, KY, Wang, Y Efficacy of pregabalin in acute postoperative pain: A meta-analysis. Br J Anaesth. (2011). 106 454–62
- 5. Khan, ZH, Rahimi, M, Makarem, J, Khan, RH Optimal dose of pre-incision/post-incision gabapentin for pain relief following lumbar laminectomy: A randomized study. Acta Anaesthesiol Scand. (2011). 55 306–12
- 6. Van Elstraete, AC, Tirault, M, Lebrun, T, Sandefo, I, Bernard, JC, Polin, B, Vally, P, Mazoit, JX The median effective dose of preemptive gabapentin on postoperative morphine consumption after posterior lumbar spinal fusion. Anesth Analg. (2008). 106 305–8
- 7. Buvanendran, A, Kroin, JS, Della Valle, CJ, Kari, M, Moric, M, Tuman, KJ Perioperative oral pregabalin reduces chronic pain after total knee arthroplasty: A prospective, randomized, controlled trial. Anesth Analg. (2010). 110 199–207