Advances in Musculoskeletal Ultrasound Technology
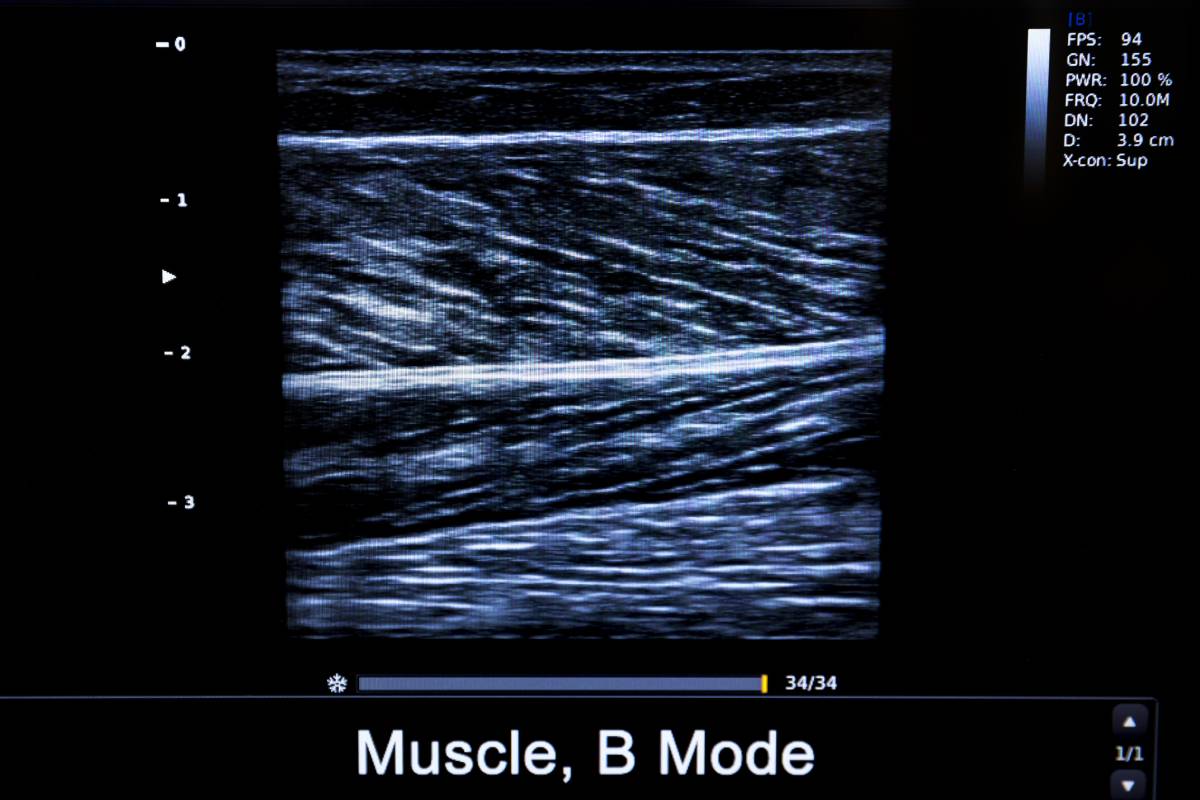
The intellectual output of an engineer-obstetrician duo, ultrasound was first used clinically as a medical imaging technology in 1956, becoming commonplace in the 1960’s, and has since established itself as a cornerstone medical imaging procedure. Key advantages over other imaging modalities include its low cost of manufacturing and use, noninvasive nature, easy visualization of hemodynamics and tissue properties, compatibility with real-time dynamic assessment, and ease of use in the form of portable ultrasound devices 1. Recently, a number of advances in musculoskeletal ultrasound imaging, in particular, have galvanized its use across multiple clinical applications 2.
First, Doppler ultrasound has been critical for the diagnosis and monitoring of inflammatory arthropathies and the assessment of neoplasms, tendinopathies, and neuropathies. For example, Doppler ultrasound can differentiate between active synovitis and chronic fibrotic synovium, as the former appears as hyperemia 3, and, in oncologic imaging, can clearly distinguish benign from malignant tumors 4.
However, traditional Doppler ultrasound remains limited by its inability to clearly visualize microvascular flow, since its algorithm filters lower velocity elements to reduce clutter. Clearly assessing microvascular flow is key, though, to diagnosing early inflammatory processes and neoplastic angiogenesis 4,5. To this end, multiple advanced ultrasound methods have been developed. First, contrast-enhanced ultrasound, combining microbubble-based intravenous contrast agents with traditional ultrasound, can, unlike previous Doppler ultrasound methods, display blood perfusion and identify capillary-level neovascularization 6. Second, another distinct Doppler technique, incorporating a unique motion suppression algorithm that isolates and eliminates clutter, can also enable the visualization of low flow microvasculature 7.
Most recently, ultra-high frequency transducers, reaching frequencies of 20-70 MHz, far exceeding the traditional 12-18 MHz range, have also been used to visualize increasingly granular anatomical detail. As such, individual fascicles may now be distinguished using the newest high-frequency ultrasound technology 8. Clinically, this first means that ultrasound-guided neurosurgical procedures can spare nerve fascicles, presenting clear advantages over conventional ultrasound or magnetic resonance imaging 9. Second, various musculoskeletal features can be accurately measured. Tendons are easily seen, thereby enabling, for example, the identification of pulleys during ultrasound-guided treatments, resulting in safer surgeries 10. Capsular ligaments, retinacula, and fasciae, all involving millimeter-diameter mesenchymal structures, are now also distinctly visible 2. Finally, this new level of precision means that ultrasounds can be used for the early detection of neoplastic masses several millimeters in size. Importantly, however, as the frequency of the ultrasound beams increase, penetration decreases. Thus, these ultrahigh frequency transducers are best suited for assessing for superficial structures.
Finally, elastography can now be used to investigate and possibly heal musculoskeletal system function. To this end, assessing stiffness of nerves and tissue around nerves in fibro-osseous tunnels can be done either by traditional strain or shear-wave elastography techniques 11.
Ultrasound is less physically and economically demanding on patients and has been greatly improving the quality of medical care. Given the rapidity of advances in ultrasound technologies, there is a clear need to standardize the execution and reporting of different associated techniques. Nonetheless, ultrasound continues to represent an indispensable diagnostic imaging modality in clinical settings, with likely many exciting additional future prospects.
References
1. Matsuzaki M. The latest technology of musculoskeletal ultrasonography: iterative revolution. J Med Ultrason. 2017. doi:10.1007/s10396-017-0799-0
2. van Holsbeeck M, Soliman S, van Kerkhove F, Craig J. Advanced musculoskeletal ultrasound techniques: What are the applications? Am J Roentgenol. 2021. doi:10.2214/AJR.20.22840
3. Aggarwal R, Aggarwal V. High-Resolution musculoskeletal ultrasound in India: The present perspective and the future. Indian J Rheumatol. 2018. doi:10.4103/0973-3698.238196
4. Jiang Z Zhen, Huang Y Hua, Shen H Liang, Liu X Tian. Clinical Applications of Superb Microvascular Imaging in the Liver, Breast, Thyroid, Skeletal Muscle, and Carotid Plaques. J Ultrasound Med. 2019. doi:10.1002/jum.15008
5. Arslan S, Karahan AY, Oncu F, Bakdik S, Durmaz MS, Tolu I. Diagnostic performance of superb microvascular imagingand other sonographic modalities in the assessment of lateral epicondylosis. J Ultrasound Med. 2018. doi:10.1002/jum.14369
6. Qin S, Caskey CF, Ferrara KW. Ultrasound contrast microbubbles in imaging and therapy: Physical principles and engineering. Phys Med Biol. 2009. doi:10.1088/0031-9155/54/6/R01
7. Yokota K, Tsuzuki Wada T, Akiyama Y, Mimura T. Detection of synovial inflammation in rheumatic diseases using superb microvascular imaging: Comparison with conventional power Doppler imaging. Mod Rheumatol. 2018. doi:10.1080/14397595.2017.1337288
8. Cartwright MS, Baute V, Caress JB, Walker FO. Ultrahigh-frequency ultrasound of fascicles in the median nerve at the wrist. Muscle and Nerve. 2017. doi:10.1002/mus.25617
9. Forte AJ, Boczar D, Oliver JD, Sisti A, Clendenen SR. Ultra-high-frequency Ultrasound to Assess Nerve Fascicles in Median Nerve Traumatic Neuroma. Cureus. 2019. doi:10.7759/cureus.4871
10. Yang TH, Lin YH, Chuang BI, et al. Identification of the Position and Thickness of the First Annular Pulley in Sonographic Images. Ultrasound Med Biol. 2016. doi:10.1016/j.ultrasmedbio.2015.12.007
11. Ooi CC, Malliaras P, Schneider ME, Connell DA. “Soft, hard, or just right?” Applications and limitations of axial-strain sonoelastography and shear-wave elastography in the assessment of tendon injuries. Skeletal Radiol. 2014. doi:10.1007/s00256-013-1695-3